The Quest For Ways To Painless Death: A Detailed Guide
The Search for Painless Death: A Comprehensive Exploration
Does the right to a dignified life extend to the right to a dignified death? The quest for "ways to painless death" is not a morbid fascination but a profound exploration of what it means to face mortality with grace and minimal suffering. This concept has fueled contemplation, spurred research, and ignited intense debate throughout history, encompassing diverse methods and approaches aimed at minimizing or eliminating pain and suffering during the final chapter of life.
The significance of painless death lies in its potential to offer a dignified and humane exit for individuals grappling with terminal illnesses or unbearable pain. It brings solace and peace of mind not only to the dying person but also to their loved ones who witness their struggle. Throughout history, societies have wrestled with the complex ethical and legal dimensions of assisted dying, euthanasia, and other means of achieving a peaceful and painless death.
- Unlock Kosta Kecmanovic Video What To Watch Why It Matters Now
- What Happened Erin Olash Onlyfans Leak Scandal Explained Aftermath
| Aspect | Details |
|---|---|
| Historical Context | Societies throughout history have grappled with end-of-life decisions, often influenced by cultural and religious beliefs. |
| Current Debate | Modern debates revolve around patient autonomy, the role of medical professionals, and legal frameworks for assisted dying. |
| Key Arguments | Proponents emphasize the right to self-determination and relief from suffering; opponents raise concerns about the sanctity of life and potential abuse. |
| Global Variations | Laws and practices vary significantly across countries and regions, reflecting diverse ethical and cultural perspectives. |
| Future Directions | Ongoing research and dialogue aim to develop compassionate and ethical approaches to end-of-life care. |
The pursuit of painless death encompasses various dimensions, each offering unique insights into the complexities of end-of-life care. Six key aspects merit exploration:
- Medical Intervention: Palliative care, pain management, and assisted dying.
- Legal Frameworks: Euthanasia, physician-assisted suicide, and advance directives.
- Ethical Considerations: Autonomy, beneficence, and the sanctity of life.
- Cultural Perspectives: Religious beliefs, societal norms, and attitudes towards death.
- Technological Advancements: Artificial intelligence, virtual reality, and personalized medicine.
- Psychological Support: Counseling, therapy, and emotional support for patients and families.
These aspects are interconnected and influence the way societies approach painless death. Medical interventions provide physical relief, while legal frameworks establish boundaries and safeguards. Ethical considerations guide decision-making, ensuring respect for individual autonomy and well-being. Cultural perspectives shape societal attitudes and influence policy development. Technological advancements offer new possibilities for pain management and end-of-life care. Psychological support addresses the emotional and mental challenges faced by patients and their loved ones.
Medical intervention plays a crucial role in achieving painless death by alleviating suffering and providing comfort during the end-of-life process. Palliative care focuses on managing pain, symptoms, and emotional distress through a holistic approach that involves medical treatment, therapies, and emotional support.
- Exploring Donnie Van Zant The Legacy Of A Southern Rock Icon
- Breaking Gabe Watson And Kim Lewis Are They Still Together Find Out
- Palliative Care:
Palliative care represents a cornerstone in the pursuit of painless death. It strives to enhance the quality of life for patients facing life-limiting illnesses by meticulously managing pain, addressing debilitating symptoms, and providing unwavering psychological support. A multidisciplinary team of healthcare professionals collaborates to deliver comprehensive physical, emotional, and spiritual care to both patients and their families. This approach recognizes that end-of-life care extends beyond mere physical comfort, encompassing the emotional and spiritual well-being of all involved.
- Pain Management:
Pain management stands as a critical pillar within palliative care, employing a diverse array of medications, therapeutic interventions, and advanced techniques to alleviate pain and discomfort. This encompasses a spectrum of approaches, from traditional pain relievers to nerve blocks that interrupt pain signals, and alternative therapies like acupuncture and massage, which offer complementary relief. The goal is to tailor a pain management plan that addresses the specific needs and preferences of each patient, ensuring they experience the greatest possible comfort.
- Assisted Dying:
Assisted dying, often referred to as euthanasia or physician-assisted suicide, represents a highly debated yet increasingly considered medical practice. It involves a physician intentionally ending a patient's life at their explicit request, driven by the desire to alleviate unbearable suffering when all other options have been exhausted. This practice remains fraught with ethical and legal complexities, sparking passionate debates about individual autonomy, the role of medical professionals, and the sanctity of life.
These medical interventions offer varying levels of pain relief and control, depending on the patient's condition and preferences. Palliative care provides comprehensive support and comfort, while pain management focuses specifically on alleviating physical discomfort. Assisted dying, though ethically and legally complex, provides a way for patients to end their lives with dignity and minimal suffering.
Legal frameworks play a critical role in shaping the landscape of painless death by establishing the boundaries and safeguards for end-of-life decision-making. These frameworks encompass euthanasia, physician-assisted suicide, and advance directives, each with its own legal and ethical considerations.
- Euthanasia
Euthanasia, also known as mercy killing, is the intentional termination of a patient's life by a physician at their request to relieve unbearable suffering. It is legal in a handful of countries, including the Netherlands, Belgium, and Canada, under strict criteria and safeguards. The Netherlands, for instance, permits euthanasia for individuals experiencing unbearable suffering with no prospect of improvement, requiring multiple medical evaluations and psychological assessments to ensure the patient's decision is informed and voluntary.
- Physician-Assisted Suicide
Physician-assisted suicide involves a physician providing a patient with the means to end their own life, such as a lethal dose of medication. It is legal in several US states and a few other countries, with varying regulations and eligibility criteria. Oregon's Death with Dignity Act, for example, allows terminally ill adults to request a prescription for medication to end their lives, provided they meet specific criteria, including a prognosis of six months or less to live and the ability to make informed decisions.
- Advance Directives
Advance directives are legal documents that allow individuals to express their wishes regarding their end-of-life care, including decisions about medical treatment and life-sustaining interventions. These directives can help ensure that a patient's wishes are respected, even if they are unable to communicate them directly. A living will, for instance, allows individuals to specify the types of medical treatment they wish to receive or refuse in the event they become incapacitated, ensuring their autonomy is respected even when they cannot speak for themselves.
These legal frameworks provide a structured approach to end-of-life decision-making, ensuring that patients' rights and autonomy are protected while balancing the ethical and societal implications of assisted dying. They offer individuals the option to control the manner and timing of their death, reducing the likelihood of prolonged suffering.
Ethical considerations play a pivotal role in shaping the landscape of painless death. Three key ethical principlesautonomy, beneficence, and the sanctity of lifeserve as guiding principles for end-of-life decision-making.
Autonomy emphasizes the patient's right to make choices about their own body and medical treatment, including the decision to end their life. Beneficence obligates healthcare professionals to act in the best interests of the patient, which may include providing treatments to alleviate suffering or supporting the patient's decision to die with dignity. The sanctity of life principle holds that human life is inherently valuable and should be preserved whenever possible.
Balancing these principles can be challenging in the context of painless death. While respecting patient autonomy is paramount, healthcare professionals must also consider the potential consequences of assisted dying and ensure that the patient's decision is truly informed and voluntary. Beneficence requires that healthcare professionals provide compassionate care and alleviate suffering, but it may also involve supporting the patient's choice to end their life if their pain is unbearable and their quality of life is irreparably compromised.
The sanctity of life principle presents a further ethical challenge, as it raises questions about the morality of intentionally ending a human life. However, proponents of painless death argue that it can be a humane and compassionate response to intolerable suffering, and that it respects the patient's autonomy and dignity.
Navigating these ethical considerations requires careful deliberation and a nuanced understanding of the patient's circumstances and values. By engaging in open and compassionate dialogue, healthcare professionals and patients can work together to make end-of-life decisions that are ethically sound and respectful of the patient's wishes.
Cultural perspectives play a significant role in shaping societal attitudes towards death and influencing the way painless death is perceived and practiced. Religious beliefs, societal norms, and individual attitudes can all impact end-of-life decisions and the availability of painless death options.
- Religious Beliefs:
Religious beliefs can strongly influence attitudes towards painless death. Some religions, such as Buddhism and certain Christian denominations, may view death as a natural part of life and accept the practice of euthanasia or physician-assisted suicide under certain circumstances. Other religions, such as Catholicism and Orthodox Judaism, generally oppose euthanasia, believing that life is sacred and should be preserved at all costs. Within Buddhism, for example, the concept of a "good death" emphasizes a peaceful and mindful transition, which may lead some Buddhists to accept assisted dying as a means of minimizing suffering and promoting a more tranquil passing.
- Societal Norms:
Societal norms and cultural values can shape public opinion and policy regarding painless death. In societies that emphasize individual autonomy and personal choice, there may be greater acceptance of euthanasia and physician-assisted suicide. Conversely, in societies that prioritize the sanctity of life and family values, these practices may be met with more resistance. In Western cultures, for instance, the emphasis on individual rights and self-determination has contributed to a more open discussion about end-of-life choices, while in some Eastern cultures, familial obligations and community harmony may take precedence, leading to a more cautious approach.
- Attitudes Towards Death:
Individual attitudes towards death can also influence the acceptance of painless death. Some people may view death as a frightening or taboo subject, while others may embrace it as a natural part of life. These attitudes can affect personal decisions about end-of-life care and the willingness to consider painless death options. Individuals who have witnessed prolonged suffering in their loved ones may be more inclined to consider painless death options as a means of preventing similar experiences, while those who fear the unknown or hold strong beliefs about the afterlife may be more resistant to such choices.
Cultural perspectives are complex and multifaceted, and their influence on painless death can vary widely. By understanding the diverse cultural factors at play, healthcare professionals and policymakers can better address the ethical and social implications of painless death and develop policies that are sensitive to the beliefs and values of different communities.
Technological advancements are transforming the landscape of medicine, offering new possibilities for pain management and end-of-life care. Artificial intelligence (AI), virtual reality (VR), and personalized medicine are emerging as key components of ways to painless death, providing innovative solutions to alleviate suffering and improve quality of life.
AI-powered algorithms can analyze vast amounts of patient data to identify patterns and predict outcomes, enabling healthcare professionals to tailor treatments more precisely and effectively manage pain. VR technology has shown promise in providing immersive and interactive pain management interventions, such as distraction therapy and guided meditation, reducing the need for opioids and other medications. Personalized medicine approaches, which involve using genetic information to customize treatments, can optimize pain management strategies and improve overall outcomes for patients with chronic pain or life-limiting illnesses.
The integration of technological advancements into ways to painless death offers several benefits. It can enhance the accuracy and effectiveness of pain management, reduce reliance on opioids and other potentially addictive medications, and improve the overall quality of life for patients facing end-of-life challenges. As technology continues to advance, we can expect further innovations that will contribute to more humane and compassionate approaches to painless death.
Psychological support plays a crucial role in ways to painless death by addressing the emotional and mental challenges faced by patients and their families during the end-of-life journey.
- Counseling and Therapy:
Counseling and therapy provide a safe and supportive space for patients and families to process their emotions, fears, and anxieties related to death and dying. It can help them cope with grief, loss, and the practical and emotional challenges of end-of-life care. Bereavement counseling, for example, can provide families with the tools and resources they need to navigate the grieving process after the loss of a loved one, helping them cope with feelings of sadness, anger, and loneliness.
- Emotional Support:
Emotional support from family, friends, and support groups can provide a sense of comfort and belonging during a difficult time. Sharing experiences, offering empathy, and listening without judgment can help patients and families feel supported and less isolated. Support groups, in particular, can offer a valuable opportunity for patients and families to connect with others who are facing similar challenges, creating a sense of community and shared understanding.
- Spiritual Support:
Spiritual support can provide meaning and purpose during the end-of-life journey. Chaplains, spiritual counselors, or other religious figures can offer spiritual guidance, comfort, and rituals that align with the patient's beliefs and values. Spiritual rituals, such as prayer or meditation, can provide patients with a sense of peace and connection to something larger than themselves, helping them find meaning and purpose in the face of death.
- Bereavement Support:
Bereavement support helps families cope with the loss of a loved one. It can involve counseling, support groups, or other resources that provide emotional support and practical guidance during the grieving process. Estate planning assistance, for example, can help families navigate the practical and legal challenges associated with settling a loved one's affairs, reducing stress and anxiety during an already difficult time.
These psychological support services are essential components of ways to painless death, as they help patients and families navigate the emotional and mental challenges associated with end-of-life care. By providing a safe and supportive environment, counseling, therapy, and emotional support can improve quality of life, reduce distress, and promote a sense of well-being during this difficult time.
This section addresses common questions and misconceptions about ways to painless death, providing concise and informative answers.
Question 1: Is euthanasia legal?
The legality of euthanasia varies widely around the world. In some countries, such as the Netherlands and Belgium, euthanasia is legal under strict criteria and safeguards. In other countries, it is illegal or only permitted in certain circumstances, such as physician-assisted suicide. Switzerland, while not explicitly legalizing euthanasia, allows assisted suicide under certain conditions, reflecting a more permissive approach than many other nations.
Question 2: What are the ethical considerations surrounding ways to painless death?
Ways to painless death raise complex ethical considerations, including the patient's right to autonomy, the principle of beneficence (doing good), and the sanctity of life. Balancing these principles requires careful deliberation and a nuanced understanding of the patient's circumstances and values. Religious and philosophical perspectives also play a crucial role in shaping ethical viewpoints, with some traditions emphasizing the inherent value of life regardless of suffering, while others prioritize individual choice and the relief of pain.
Understanding the legal and ethical aspects of ways to painless death is crucial for informed decision-making. These practices are subject to ongoing debate and legal scrutiny, and it's essential to stay informed about the latest developments and regulations in your jurisdiction. The legal landscape is constantly evolving, with new court cases and legislative initiatives shaping the future of end-of-life care.
The exploration of ways to painless death has illuminated the complex interplay of medical advancements, legal frameworks, ethical considerations, cultural perspectives, technological innovations, and psychological support. This multifaceted approach recognizes the unique needs and preferences of individuals facing end-of-life decisions.
As societies continue to grapple with the ethical and legal implications of painless death, ongoing dialogue and research are essential. By fostering a compassionate and informed understanding, we can strive to ensure that individuals have access to dignified and humane end-of-life options that align with their values and beliefs. This includes supporting initiatives that promote palliative care, improve pain management, and provide access to psychological and spiritual support for patients and their families.
- Rumor Mill Hailey Van Lith Boyfriend 2024 Truth Amp Privacy
- Is Jyoti Amge In A Relationship What We Know 2024

Recognizing the Signs of Suicide and How You Can Help CropWatch
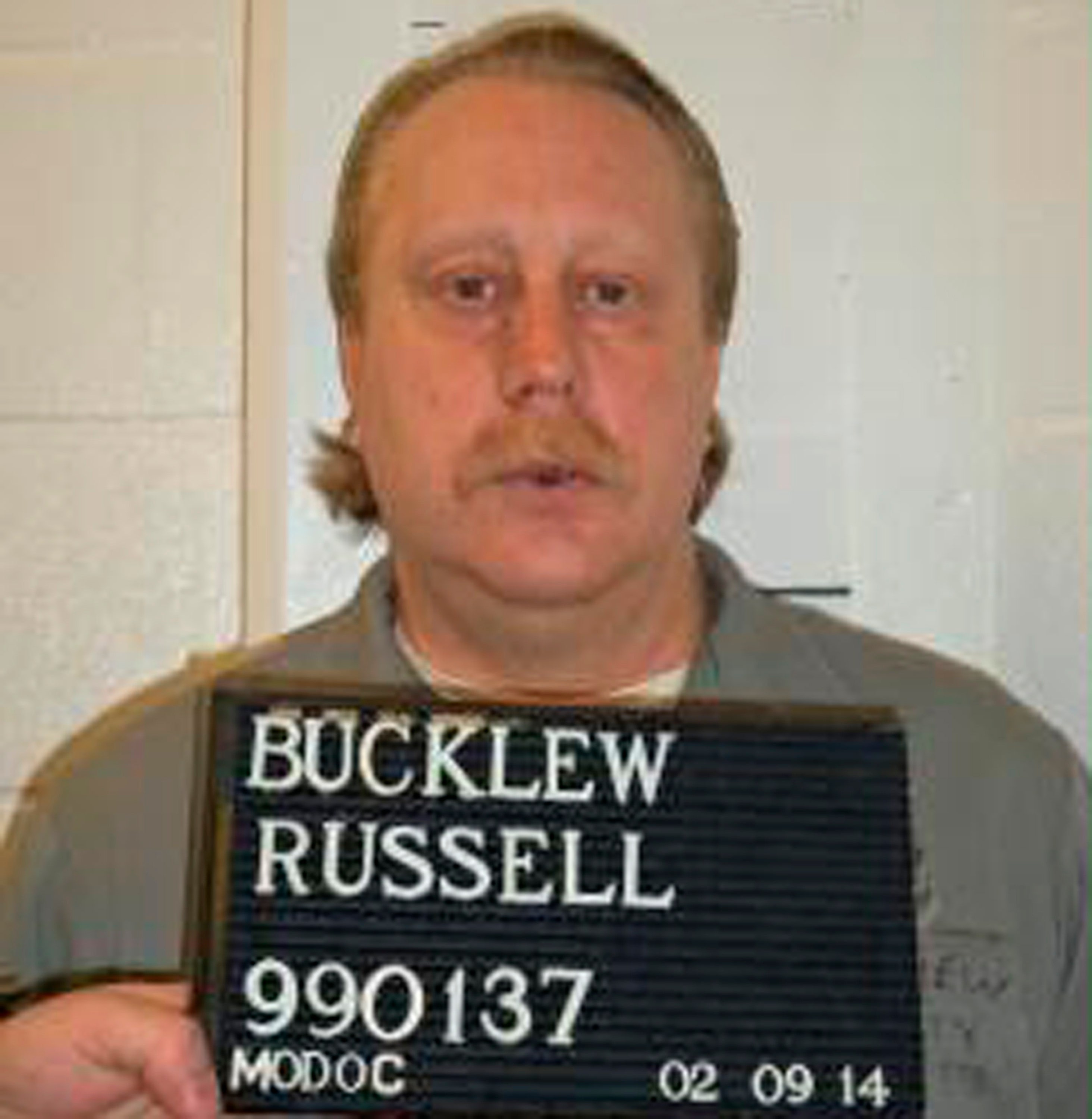
Supreme Court, Gorsuch rule Missouri inmate with disease has no right

What's the best method for a painless suicide?